Age-related macular degeneration is the most common cause of damage to one’s central vision.
We are constantly using our eyes, whether watching TV, looking at our latest electronic gadget, driving, reading or simply relaxing. It is easy to take good eyesight for granted, and even easier to assume that difficulty in vision is simply due to a change in one’s glasses prescription. However, 15 million Americans—and millions more around the world—suffer from age-related macular degeneration (AMD), which damages a part of our eyes called the macula, making even mundane tasks very challenging.
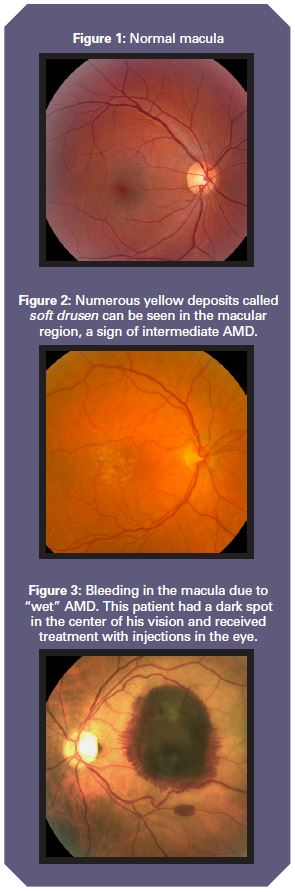
The retina is nerve tissue which lines the inside of our eyes like a carpet. The central part of the retina—about the size of a pinhead and densely packed with light-sensing nerve cells—is the macula, which provides us with central or straight-ahead vision, as well as color vision (See Figure 1). The rest of the retina is responsible for peripheral or side vision, such as looking out of the corner of your eye.
 How Prevalent is AMD?
How Prevalent is AMD?
AMD is the most common cause of vision loss and legal blindness in the U.S. Overall, three million Americans will have advanced AMD by 2020. More than one in three senior citizens over the age of 75 currently have signs of macular degeneration, with approximately 200,000 new cases diagnosed each year.
The risk of AMD increases dramatically with age. Additional risk factors include: female sex, Caucasian race, blue eyes, positive family history, AMD in the other eye, smoking, a diet high in saturated fats and low in antioxidants, high cholesterol, obesity, a sedentary lifestyle, and high blood pressure.
Types of AMD
The condition always starts out as “dry” AMD, with tiny yellow deposits called drusen forming over the macula. Small, discrete or “hard” drusen are common and may not affect vision. However, more than seven million Americans have large or soft drusen (See Figure 2) and are at risk of progression to advanced AMD.
Dry AMD can result in the loss of central or reading vision due to the loss of tissue over the macula. However, 90 percent of cases of legal blindness from AMD are due to the “wet” form, in which abnormal blood vessels form under the macula and cause leakage of fluid or bleeding (See Figure 3). Eventually, blood causes scarring in the macula, leading to the permanent loss of vision. “Wet” AMD almost never starts out as “wet.” Rather, it develops on the back of dry AMD.
Symptoms of AMD
The early stages of AMD often arrive without symptoms. Intermediate AMD (soft drusen) may also be asymptomatic, or it may be associated with a slight blurring, distortion or decline in vision. AMD does not cause pain or redness in the eye.
Unlike the ears, both of our eyes are pointed straight ahead at the same object. Therefore, a painless condition such as AMD affecting only one eye may not be detected by the patient, due to the other eye subconsciously taking over. With advanced AMD (atrophy or wet AMD), a dark or black spot develops in the center of one’s vision.
How is AMD diagnosed?
It is important for all of us to check our vision in each eye by reading or watching TV after covering the other eye for at least five minutes daily, and report any new distortion, blurriness or a dark spot to your eye care provider. An examination of the back of the eye after the dilation of pupils, combined with other special tests, is required for an accurate diagnosis.
Treatment of AMD
Intermediate cases of dry AMD are treated with vitamins that can slow down (but not completely stop) its progression. The most effective treatment of wet AMD involves the injection of medications into the eye. It is important to note that these injections do not “cure” wet AMD, but only manage to control it. Approximately 90 percent of patients can expect to stabilize their vision with repeated injections. Those who are diagnosed early and have smaller areas of damage do better.
AMD is the most common cause of damage to one’s central vision. Awareness of its symptoms and daily monitoring of vision by alternately covering one eye, then the other, may uncover its symptoms at an earlier stage. Early detection and prompt treatment are associated with improved outcomes. iBi
Kamal Kishore, MD, is a fellowship-trained retina specialist at Illinois Retina & Eye Associates.


